Connect With Us
Featured Articles
Items filtered by date: February 2022
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Where Heel Pain Can Come From
 Heel pain can be debilitating and have a brutal impact on everyday life. While there are a variety of causes of heel pain, the most common is plantar fasciitis. This happens when there is inflammation or even a partial tear in the tissue running along the bottom of the foot that connects the heel to the toes, known as the plantar fascia. Heel pain can also occur when there is an abnormal growth on the heel bone that is a result of a calcium buildup. This is known as a heel spur. Other common sources of heel pain include Calcaneal apophysitis (irritation of the heel bone from new shoes or a new activity), bursitis (inflammation of the sac that lines some joints), or when a nerve gets compressed (also known as a trapped nerve). If you are struggling with heel pain, consulting with a podiatrist is a good idea. A podiatrist will be able to find the cause of the heel pain and suggest the treatment options that are available.
Heel pain can be debilitating and have a brutal impact on everyday life. While there are a variety of causes of heel pain, the most common is plantar fasciitis. This happens when there is inflammation or even a partial tear in the tissue running along the bottom of the foot that connects the heel to the toes, known as the plantar fascia. Heel pain can also occur when there is an abnormal growth on the heel bone that is a result of a calcium buildup. This is known as a heel spur. Other common sources of heel pain include Calcaneal apophysitis (irritation of the heel bone from new shoes or a new activity), bursitis (inflammation of the sac that lines some joints), or when a nerve gets compressed (also known as a trapped nerve). If you are struggling with heel pain, consulting with a podiatrist is a good idea. A podiatrist will be able to find the cause of the heel pain and suggest the treatment options that are available.
Many people suffer from bouts of heel pain. For more information, contact Scott Matthews, DPM, MD of Salem Foot Care . Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Wikesboro, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Vascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.
Vascular Testing to Help Determine Peripheral Arterial Disease
Some of the symptoms of peripheral arterial disease (PAD) can include pain, weakness, numbness, loss of hair on your legs, bluish-colored skin on the feet or calves, poor toenail growth, pain or cramps in your legs when walking, and wounds on your feet and legs that are slow to heal. To properly diagnose this vascular condition, your podiatrist may need to know your Ankle Brachial Index (ABI). Simply put, the ABI compares the blood pressure in the arm with the blood pressure in the ankle. Blood pressure during the heart’s contracting/pumping (systolic) phase is slightly higher in the ankle than it is in the arm for healthy people. Determining the ABI is a very simple and non-invasive procedure, using just a blood pressure cuff and a Doppler instrument. The patient lies down and rests for ten minutes. Then, blood pressure is taken at the upper arm, followed by the ankle. The ankle’s blood pressure is then divided by the arm’s blood pressure. An ABI ratio between 1.0 to 1.4 is considered normal. An ABI ratio of 0.9 or less usually indicates PAD—with moderate cases typically ranging between 0.4 to 0.7, and more severe cases falling below 0.4. If you are experiencing any symptoms of PAD, contact a podiatrist right away for a full examination and to see if your ABI should be analyzed.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with Scott Matthews, DPM, MD from Salem Foot Care . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact our office located in Wikesboro, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
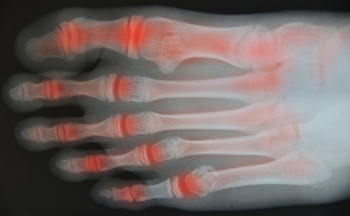
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
A PSA About PsA
Psoriatic arthritis, commonly abbreviated as PsA, is a form of arthritis that affects people who have a skin condition called psoriasis – although people without psoriasis can get it, too. PsA causes many of the joint symptoms associated with other types of arthritis, including pain, swelling, stiffness, and reduced mobility. More unique to PsA are symptoms such as toenail pitting, discoloration, and detachment, toe swelling, and itchy skin. If you have any type of arthritis affecting the lower limbs, a podiatrist can help you maintain or improve your foot and ankle health and mobility. To learn more about PsA and how to properly care for arthritic feet, please consult with a podiatrist.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Scott Matthews, DPM, MD from Salem Foot Care . Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Wikesboro, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Extensor Tendonitis May Cause Pain in the Top of Your Foot
Pain in the top of the foot can be caused from a variety of conditions, one of them being extensor tendinitis. Tendons are fibrous tissues that connect muscles to bone. Extensor tendons are located on the top of the feet. They connect bones in the toes to muscles on the front portion of the leg which work together to help raise your toes and flex your feet. These tendons can become inflamed and irritated from wearing tight, small, or non-supportive shoes, or from overuse. This condition, known as extensor tendonitis, can cause pain and swelling in the top of the feet that may worsen after activity. If you are experiencing this type of foot pain, it is a good idea to contact a podiatrist. After the examination, if it’s determined that you have extensor tendonitis, your doctor may prescribe a course of treatment that includes rest, anti-inflammatory medication, splinting, physical therapy, or even steroid injections.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Scott Matthews, DPM, MD from Salem Foot Care . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Wikesboro, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.